I would like to share with you some important developments in the field of orofacial and dental development that could have a profound impact on our patient’s general health.
There is mounting evidence that malocclusion has become more prevalent in our modern societies (1-6). Like height and weight, our face and occlusion develop over a period of time and is highly influenced by the environment and our behaviors. Well recognized behavior problems such as thumb-sucking and mouth-breathing cause very specific patterns of malocclusion. On the contrary, there is no report that any infant is born with a skeletal Class III malocclusion. Malocclusion is always developed over time and subject to environmental stimulus.
The important stimuli that can shape the development of the maxilla and mandible includes mode of breathing, pattern of swallowing, and mastication. These factors also influenced the formation of our occlusion. The pattern of breathing and swallowing are established very early during the infant stage when mammals fine tune these vital reflexes during breastfeeding (7). Unfortunately, in modern society, people often interfere with this important developmental process with bottle feeding and/or pacifiers.
A transition from hunter-gather to agriculture lifestyle coincided with a reduction in the size of our craniofacial dimensions (8-11). The modern softer diet reduces demand on our mastication muscles and subsequently less stimulus for the bone development occurs to both the maxilla and mandible. Prevalence of allergies and poor indoor/outdoor air quality promotes higher frequency of mouth-breathing in modern city dwellers.
Mouth-breathing causes a low tongue posture, which in turn reduces the transverse development of the maxilla (12). Tongue-thrust swallowing pattern and overactive orbicularis oris muscles are always observed in patients with dental crowding and/or excessive overbite.
Malocclusion is simply a sign that the maxilla and mandible have not developed normally, and it is caused by a combination of genetics and abnormal functions such as mouth-breathing, tongue-thrust swallowing pattern, and inappropriate action of mastication muscles. Myofunctional therapy needs to be included as a part of orthodontic treatment to correct these abnormal functions.
The following examples showcase abnormal function and corresponding malocclusion.
Case 1: Severe dental crowding and posterior crossbite of a chronic mouth-breather.

Case 2: Active lower lip during swallowing and corresponding lower anterior crowding.

Case 3: Lateral tongue-thrust pattern and mirrored dental misalignment.

When there is underdevelopment of the maxilla and mandible, the most serious impact is not the ability to masticate but rather the airway (19-22). The roof of mouth is the same anatomical structure as the floor of nose and their development is obviously intimately linked. The nasopharyngeal airway is situated right behind the maxilla. Underdevelopment of the maxilla logically implies a more constricted nasal passage (13) and nasopharyngeal airway. Behind the mandible is our tongue and behind the tongue is our oropharyngeal airway. A retrognathic or constrict mandible can easily cause the tongue to encroach on the oropharyngeal airway. A compromised airway is a serious health problem for our patients. A patient who has significant malocclusion due to underdevelopment of the maxilla and/or mandible should also be screened for potential airway constriction and breathing issues.
The good news is that behaviors, unlike genetic factors, can be modified. This points to the importance of early screening and intervention. Studies have shown orthodontic treatment such as maxillary expansion can be effective in treating pediatric sleep apnea (14). Mandibular advancement appliances have also been recognized as an effective treatment method for obstructive sleep apnea (15). Arch expansion and forward development of the maxilla and mandible should be the primary treatment of choice when dealing with malocclusion because these strategies can positively impact the airway and improve our patient’s health. Total airway volume is increased after maxillary expansion with an average airway expansion of +11.54% (2.35 % increase per mm expansion) (16).
The conventional treatment of serial extraction is designed to guide the eruption of the permanent anterior teeth, but it does not taken into account the facial growth and therefore does not provide any benefit for the airway development. Extraction does not address the etiology of malocclusion such as abnormal oral functions. A couple of recent studies link missing teeth with an increased risk of developing obstructive sleep apnea/OSA (17). The risk of developing OSA correlated positively to the number of tooth loss (2% increase in risk for every tooth loss). People who lose their teeth also had greater odds in developing OSA as they age. Thus the breathing and associated health problems get worse as these individuals grow older.
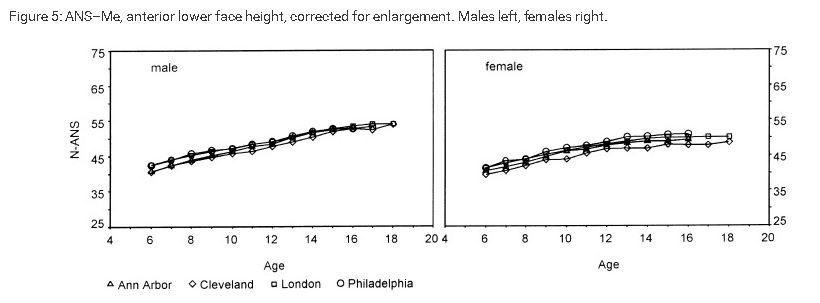
Treating patients in the early primary dentition or earlier seems to achieve the most favorable response in terms of the arch expansion and forward facial development. The reason is that certain dimensions of facial development complete a lot earlier than the somatic development. The cranium size is 90 percent complete by age six to eight. Cephalometric tracing from various orthodontic growth centers show the lower anterior facial height on average is about 70 to 80 percent completed by age six (Fig 1). The mandible is developing fastest in the first year of our life then slows down gradually as we get older (18).
Fig 1. Orthodontics and Craniofacial Research 5(1):51-8 · March 2002
When treating patients in the conventional 12 to 14 years age or later, on average, there is minimal facial growth potential left for positive skeletal modification. We can still straighten teeth but it is often not possible to predictably correct the skeletal deficiency and it is very difficult to improve the airway (with the exception of bi-maxillary advancement orthognathic surgery).
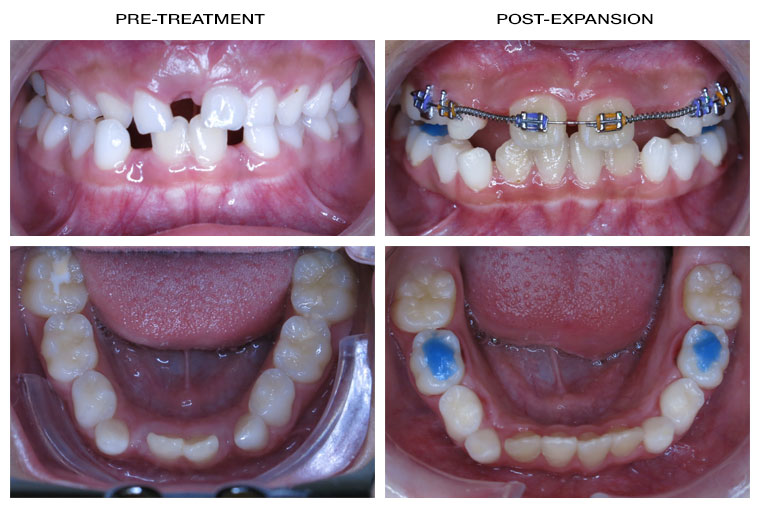
It has been taught in dental school that the mandible cannot be expanded or modified. The following cases will demonstrate that the lower arch can be expanded to correct most dental crowding problems provided that the problem is intercepted early on. I deployed a physiological expansion method that accounted for the rate of PDL remodeling. Average expansion rate is 1 mm per month. Notable benefits from the early treatment with expansion and functional appliance are the positive development of the face, body posture, and improvement of the airway.
Case 1-2. Expansion to correct severe lower arch space deficiency hence avoid serial extraction.
Case 1: expansion to allow eruption of 3.2. and 4.2.
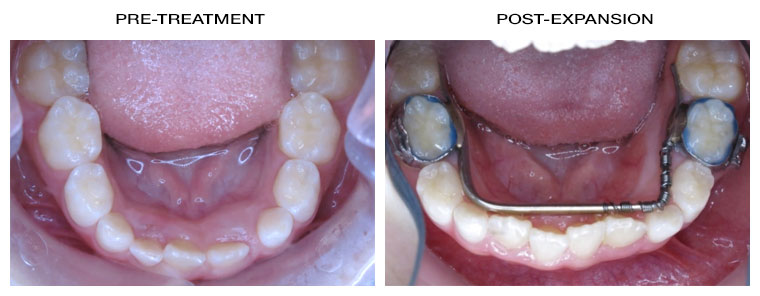
Case 2: 3.2. Severe upper and lower crowding and constricted maxilla.
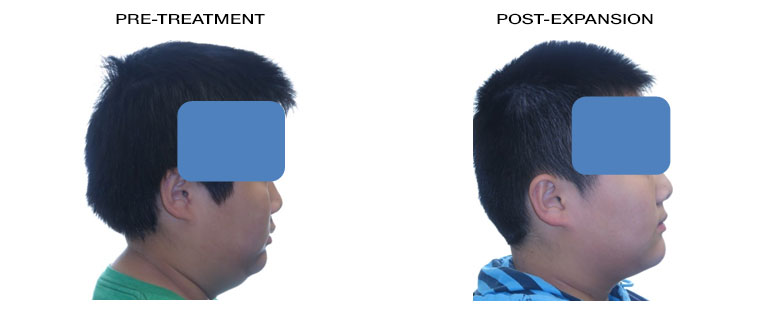
Case 3-5: Facial and posture improvement after expansion and functional appliance treatment.
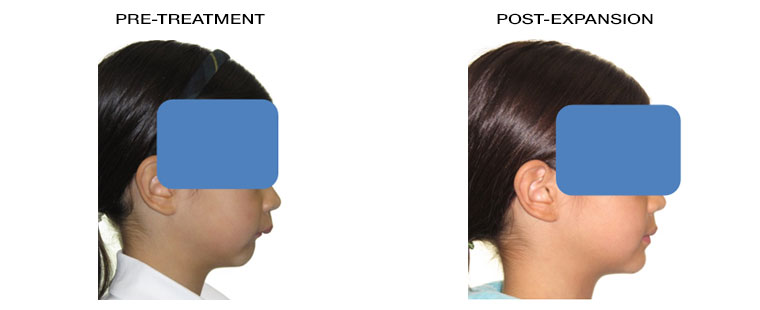
Case 3: Forward facial development of maxilla and mandible after expansion of dental arches.
Case 4: Improved head posture and lip competency in ten months. Note the change in her neck curvature; patient changed from a head forward posture to a better neutral head position. This indicates an improvement in airway which results in less positional compensation required by the patient.
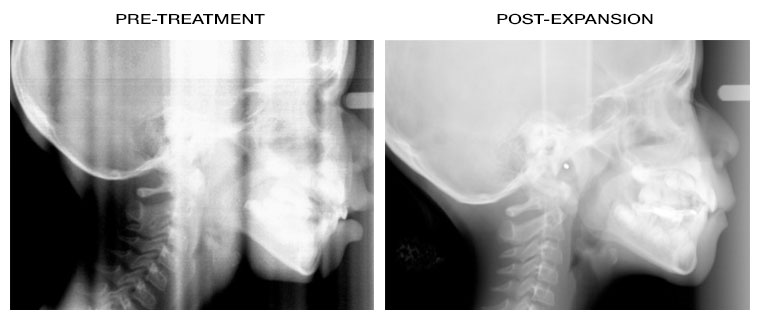
Case 5: Long term thumb-sucking resulted in an extreme retrognatahic mandible. Forward growth of the mandible with mandibular advancement appliance in 12 months.
Realistically, treatment can start when a patient is 6+ years old. I highly recommend early screening to diagnose potential growth and development issues. Early intervention can result in the best growth response. Please do not hesitate to contact me if you would like to learn more about the orthodontic treatment options that have the potential to make the face grow more favourably as well as improve our most important function — breathing.
Yours sincerely,
Brian P.L. Hong, D.D.S., FRCDC
Certified Specialist in Orthodontics
Scientific References:
(1) Am. J. Hum. Genet. 19(4):543. 1967.
(2) J. Hum. Lact. 14(2):93. 1998
(3) 7:343. 1962
(4) Brash, J.C.: The Aetiology of Irregularity and Malocclusion of the Teeth. Dental Board of the United Kingdom, London, 1929.
(5) Robert S. Corruccini, AJO-OD. 86(5):419
(6) Odonto-Stomatologie Tropicale. 90:25.
(7) Barlow SM1 Central pattern generation involved in oral and respiratory control for feeding in the term infant. Curr Opin Otolaryngol Head Neck Surg. 2009 Jun;17(3):187-93.
(8) Goodman AH, (1984) Diet and post Mesolithic craniofacial and dental evolution in Sudanese Nubia. Science in Egyptology, (Manchester Univ Press, Manchester, UK), pp 201–210.
(9) Kaifu Y (1997) Changes in mandibular morphology from the Jomon to modern periods in eastern Japan. Am J Phys Anthropol 104:227–243.
(10) Sardi ML, (2006) Craniofacial morphology in the Argentine Center-West: Consequences of the transition to food production. Am J Phys Anthropol 130:333–343
(11) Holmes MA, Ruff CB (2011) Dietary effects on development of the human mandibular corpus. Am J Phys Anthropol 145:615–628
(12) Harvold EP, AJO-DO 1981 Apr;79(4):359-72.
(13) Cistulli PA1, Chest. 1996 Nov;110(5):1184-8. Influence of maxillary constriction on nasal resistance and sleep apnea severity in patients with Marfan's syndrome.
(14) Pirelli P1, Rapid maxillary expansion in children with obstructive sleep apnea syndrome. Sleep 2004 Jun 15;27(4):761-6.
(15)Marla Pia Villa et al, Mandibular advancement devices are an alternative and valid treatment for pediatric obstructive sleep apnea syndrome. Sleep Breath 2012 Dec;16(4):971-6.
(16) Motro M, Rapid-maxillary-expansion induced rhinological effects. Eur Arch Otorhinolaryngol. 2016 Mar;273(3):679-87
(17-1) Guilleminault C1 , Missing teeth and pediatric obstructive sleep apnea. Sleep Breath. 2016 May;20(2):561-8
(17-2) Anne E. Sanders1, Tooth loss and obstructive sleep apnea signs and symptoms in the US population. Sleep Breath. 2016 September; 20(3): 1095–1102.
(18) Yi-Ping Liua, Mandibular Growth, Remodeling, and Maturation During Infancy and Early Childhood. Angle Orthod 2010;80:97–105
(19) Cephalometric analysis in patients with obstructive sleep apnoea syndrome. The Journal of Laryngology & Otology. Volume 103, Issue 3 March 1989 , pp. 287-292.
(20) Walter Hochban, Journal of Cranio-Maxillo-Facial Surgery. August 1994 Vol 22, Issue 4, 205–213. Morphology of the viscerocranium in obstructive sleep apnoea syndrome - cephalometric evaluation of 400 patients.
(21) Yoon-Ji Kim, Three-dimensional analysis of pharyngeal airway in preadolescent children with different anteroposterior skeletal patterns. AJO-DO, March 2010 Volume 137, Issue 3, Pages 306.
(22) Alan A. Lowe, Cephalometric and computed tomographic predictors of obstructive sleep apnea severity. , AJO-DO, June 1995Volume 107, Issue 6, Pages 589–595.
